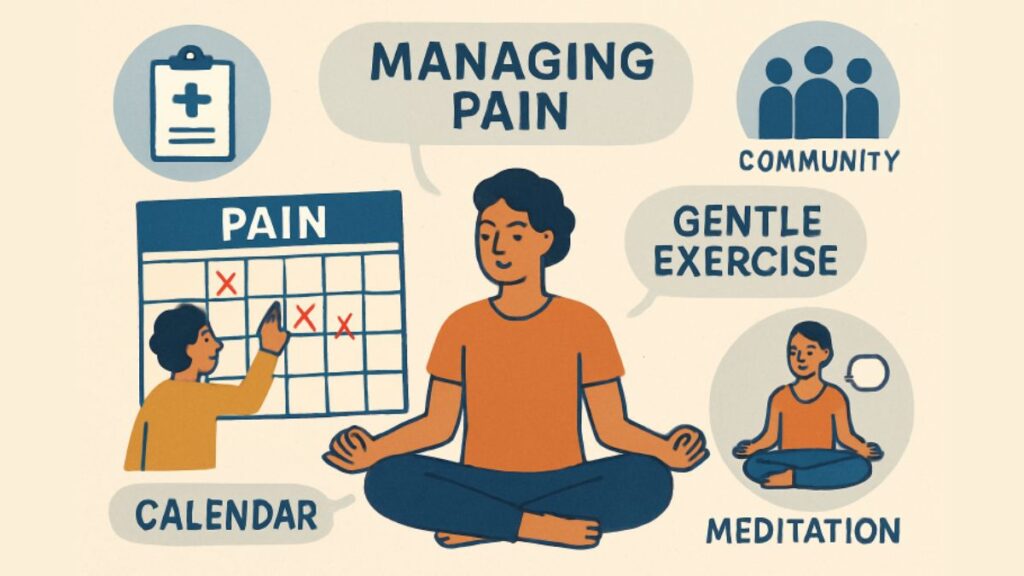
Chronic pain affects millions, demanding resilience and adaptive strategies from those who experience it. For many, finding effective relief is not simply about medication or professional intervention—it’s about embracing self-management. This proactive approach equips individuals with lifelong skills to regain control of their health, improve day-to-day functioning, and develop confidence in managing pain independently. In major metropolitan areas, seeking resources like a pain specialist in Chicago can be a crucial first step. Still, self-management takes the commitment a step further by making individuals key players in their own journeys. Self-management is not just a complement to clinical care—it’s a transformative process. Encompassing personalized exercise routines, cognitive strategies, and mindfulness, it enables people to make informed choices and adapt throughout life’s changes. By focusing on both physical and mental health, self-management offers a path for people to move from simply coping to actively thriving, even in the face of persistent discomfort. Developing these skills doesn’t happen in isolation. Collaboration with healthcare teams and involvement in peer support or community resources play substantial roles. This comprehensive support system empowers individuals with chronic pain to navigate challenges and achieve stronger outcomes. This article explores self-management through practical strategies, professional support, community engagement, and guidance for developing personalized pain care plans.
Understanding Self-Management
Self-management of chronic pain shifts the focus from being a passive recipient of care to becoming an active participant in personal health decisions. This approach involves developing new habits, monitoring symptoms, and seeking out resources and information. By committing to self-management, people with chronic pain gain tools to better cope with flare-ups, communicate effectively with care teams, and navigate daily tasks with greater ease and autonomy.
Evidence suggests that those who consistently use self-management strategies report lower pain intensity and higher quality of life. Education is foundational; understanding the underlying causes, triggers, and impacts of pain informs smarter decisions and empowers individuals to adapt over time. Major health organizations, such as the National Institutes of Health, advocate for patient-centered approaches to chronic pain that prioritize active involvement and ongoing learning.
Physical Activity and Exercise
Exercise is widely recognized as a powerful tool for managing chronic pain. Gentle movement boosts circulation, strengthens muscles, maintains flexibility, and reduces inflammation—key factors that help decrease pain over time. Low-impact activities like swimming, walking, and yoga are recommended for most people and accommodate various mobility levels and physical limitations.
Establishing a consistent exercise routine can be challenging, particularly for those who fear that activity might worsen their pain. However, research shows that gradually increasing activity under professional supervision generally leads to improved mobility and decreased pain. Tracking progress, setting attainable goals, and celebrating small victories help maintain motivation and reinforce the benefits over time.
Cognitive-Behavioral Strategies
Cognitive-behavioral therapy (CBT) introduces tools for changing unhelpful thoughts and behaviors that can amplify pain perception. Techniques such as identifying automatic negative thoughts, reframing challenges, and building stress management routines enable individuals to break the cycle of pain and emotional distress. Coping skills training, problem-solving, and pacing are vital elements of CBT-based approaches.
Many CBT programs today are accessible remotely, breaking down barriers to care and making support more widely available. Clinical studies confirm that CBT-based self-management improves pain severity, mood, and daily functioning, especially when integrated into broader pain management plans.
Mindfulness and Relaxation Techniques
Mindfulness practices bring awareness to the present moment and cultivate acceptance, helping to reduce anxiety and emotional suffering linked to chronic pain. Meditation, deep breathing exercises, and progressive muscle relaxation are commonly used techniques that can be practiced almost anywhere. Mindfulness-Oriented Recovery Enhancement (MORE) combines this awareness with cognitive skills, providing a holistic, evidence-based path to pain relief and emotional balance.
Studies in leading medical journals indicate that mindfulness lowers stress hormones, improves pain tolerance, and boosts a sense of control over health. Incorporating mindful practices into daily routines fosters resilience, making it easier to handle setbacks with compassion and adaptive coping skills.
Role of Healthcare Providers
Healthcare professionals are essential allies on the self-management journey. From primary care physicians to occupational therapists, their guidance helps patients understand diagnoses, monitor symptoms, and adapt strategies as needed. Providers collaborate with patients to establish realistic goals, recommend evidence-based interventions, and adjust care plans as needs change. This active partnership sets the stage for sustainable, long-term success in managing chronic pain.
Educational support from providers also includes connecting individuals to reputable resources, support groups, and structured pain management programs to support ongoing learning and encourage continued engagement.
Peer Support and Community Engagement
Pain can be isolating, but connecting with others who understand is a powerful antidote. Peer support groups—both in-person and online—offer safe spaces to share stories, get coping tips, and receive encouragement. Community organizations often offer workshops or events that promote social interaction while building new self-management skills.
Many participants describe peer support as transformational; beyond emotional validation, they gain practical advice on navigating healthcare, setting boundaries, and adjusting expectations. Broadening one’s support network reduces loneliness and enhances long-term commitment to self-care strategies. The U.S. Pain Foundation and similar organizations endorse community engagement as a critical factor in successful chronic pain management.
Developing a Personalized Plan
Every individual’s pain experience is unique, making personalized planning vital. Effective plans account for preferences, specific symptoms, life circumstances, and other health conditions. Collaborating with healthcare providers, individuals set short- and long-term goals, mix and match physical activity, cognitive strategies, and mindfulness, and regularly review what works best for them. This customized approach fosters adaptability and maximizes the potential for meaningful improvements in everyday life.
Tracking pain levels, successes, and setbacks helps inform future adjustments, building a sense of agency and ongoing progress. Adjusting these plans in partnership with a professional team keeps goals realistic and attainable, while empowering individuals to advocate for what they need.
Conclusion
Self-management offers hope and tangible tools for individuals living with chronic pain, transforming them from passive recipients of care to empowered, proactive managers of their own health. By integrating movement, cognitive-behavioral skills, mindfulness, and robust support systems, those with chronic pain can achieve greater control, resilience, and a higher quality of life. The journey is personal, but no one has to walk it alone—resources, professionals, and peers are there to help every step of the way.