Introduction
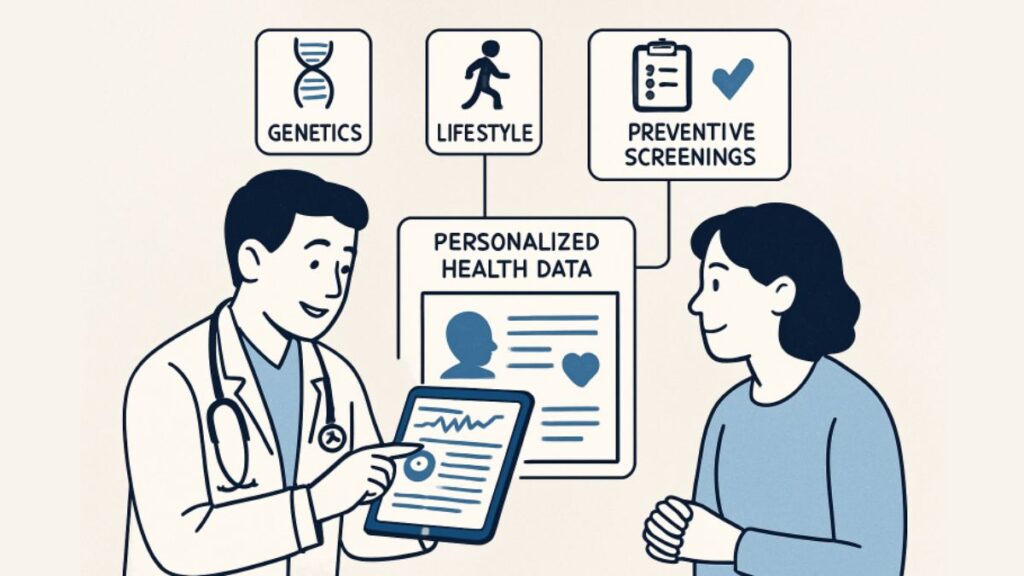
Personalized health screenings are reshaping the landscape of preventive care, enabling the detection of diseases earlier and tailoring healthcare solutions to individual needs. Unlike generic checkups, these screenings take into account each person’s family history, genetics, and lifestyle, resulting in more accurate risk assessments and timely interventions. Understanding what are diagnostic services is crucial, as these services form the cornerstone of early detection strategies, allowing healthcare providers to create a comprehensive plan that aligns with personal risk factors.
While traditional health screenings offer value, they often overlook the unique variables that can influence a person’s health trajectory. By customizing screening approaches, healthcare systems empower patients to take control of their health while optimizing resource allocation for better clinical and economic outcomes.
This trend toward personalization is driven in part by technological advancements and a growing focus on patient-centered care. In today’s digital health environment, a wide range of diagnostic and preventive services can be adapted to fit the unique needs of individuals, leading to earlier detection, more effective prevention, and improved long-term outcomes.
With chronic diseases remaining a leading cause of mortality and healthcare expenditure, the shift toward individualized screening protocols not only holds promise for patients but also offers a path to reduce unnecessary procedures and healthcare costs. As a result, both patients and providers benefit from interventions that are not only preventive but also precisely targeted.
Standardized health screenings often overlook critical risk factors, particularly in diverse populations. For instance, an individual’s risk of developing heart disease or diabetes may be underestimated if their unique genetic or lifestyle risks aren’t factored in. Personalized health screenings overcome this limitation by integrating a patient’s personal and family medical history, genetics, and everyday behaviors into a tailored assessment plan. This approach enables healthcare professionals to recommend screenings at the right intervals and with the appropriate scope, ensuring that high-risk patients receive the earliest possible interventions.
The implications go beyond early detection; personalized protocols can help identify environmental or hereditary risks that would otherwise be ignored in uniform guidelines. This transformation is already beginning to influence large-scale public health initiatives, including those targeting breast cancer screening frequency and colorectal cancer detection among various age groups and demographics. According to the CDC, tailoring screening recommendations based on individual risk results in greater efficiency and improved health equity across patient populations.
Advancements in Technology and Personalized Screenings
Technology serves as the backbone of modern personalized health screenings. Breakthroughs in artificial intelligence (AI), machine learning algorithms, and wearable health devices have significantly improved the precision and efficiency of diagnostic services. These advancements enable the continuous monitoring of physiological changes, the compilation of longitudinal health data, and the identification of patterns indicative of emerging diseases.
One such innovation comes from researchers at Carnegie Mellon University, who have used personalized models to make advances in precision cancer care—improving survival predictions and identifying subtle cancer subtypes that might have been previously overlooked. Their approach illustrates how AI-driven tools can analyze vast datasets to tailor cancer diagnostics and treatments to individual patients. These developments have exponentially expanded the diagnostic possibilities available to clinicians, enabling earlier and more specific detection.
Benefits of Personalized Health Screenings
- Early Detection: Tailored strategies significantly increase the likelihood of detecting diseases at early, treatable stages, thereby boosting survival rates and reducing the need for invasive procedures.
- Reduced Healthcare Costs: By detecting illnesses in their initial stages, healthcare systems and patients can avoid expensive acute treatments, thereby reducing both individual and societal healthcare costs.
- Improved Patient Engagement: Customized health plans foster a sense of ownership and investment in health, motivating individuals to adhere to recommended testing and preventive measures.
Additionally, patients are more likely to feel understood and supported, leading to better communication with providers and improved follow-up care—a key factor in managing chronic diseases and promoting preventive health.
Implementing Personalized Screening Programs
Healthcare organizations aiming to transition from standardized to personalized screening protocols should start by gathering comprehensive patient data. This includes details about medical history, genetics, social determinants of health, and lifestyle characteristics such as diet, exercise, and occupational exposures. Advanced predictive analytics can then be applied to assess risk and establish individualized preventive strategies.
- Aggregate detailed data from electronic health records and patient input.
- Utilize advanced analytics and risk stratification tools to customize screening recommendations.
- Establish individualized schedules for follow-ups, imaging, laboratory work, and other diagnostic procedures.
- Educate patients on their unique risks and the resulting recommended screening timeline.
Success in program implementation hinges on clear patient communication, user-friendly technology, and strong data privacy protocols. It is also important to provide ongoing training for healthcare teams on new tools and protocols to maximize adoption and effectiveness.
Challenges and Considerations
Despite the promise, personalizing health screenings introduces new complexities, including data privacy and security concerns, as well as the need for a robust technology infrastructure to support comprehensive data collection and real-time analysis. Ensuring equitable access is also critical, as disparities in access to technology or healthcare resources could widen if not carefully managed. Collaboration among healthcare providers, technology companies, and policymakers is crucial to overcoming these barriers and ensuring that advancements benefit all segments of the population. Recent discussions by the World Health Organization have underscored the importance of equity and ethical frameworks in the deployment of digital health solutions globally.
Conclusion
Personalized health screenings represent a major shift in preventive healthcare. By harnessing advanced technology and considering individual risk profiles, these programs can enhance clinical outcomes, lower healthcare costs, and empower patients to take a more proactive role in their well-being. As innovation continues, the focus must remain on overcoming challenges and expanding access to ensure that the benefits of personalized preventive care reach everyone, paving the way for healthier communities and a more efficient healthcare system overall.